Symptoms
BLADDER CONTROL PROBLEMS, INCONTINENCE
WHAT IS IT?
Urinary incontinence is when you leak urine. It may be just a few drops or larger amounts. If it happens more than once or twice a week, you may want to read this page and talk to your doctor about it.
Urinary incontinence is more common than you might think. Between 44% and 57% of middle age and postmenopausal women have some leaking. So while many women shy away from talking about it, you are not alone.
- Stress incontinence is when you leak urine when you laugh, cough, sneeze, run, exercise or lift something.
- Overactive bladder is a frequent, sudden urge to pee that may be hard to control. Waking up more than once at night needing to pee can also be overactive bladder. You can have overactive bladder without leaking urine.
- Urge incontinence is when you have a sudden urge to pee and leak urine. This can happen even right after you’ve emptied your bladder.
Incontinence can impact your quality of life. People with incontinence are more likely to have depression, low energy, and even pain. Others avoid social interactions and physical activities because of fear of leaking or needing to be close to a bathroom.
There are many options to help with incontinence. What they are depends on the underlying cause.
WHAT’S HAPPENING TO MY BODY?
First, let’s define a few things. Your bladder is a large, muscular sac that holds urine. The urethra is a muscular tube that carries urine out of the bladder when you pee. The urinary sphincter is a set of muscles around the urethra. When you urinate voluntarily the bladder muscles contract and the urethral muscles and the sphincter relax. It’s a complicated process.
As a woman ages her urethra, shortens and the mucus in it thins. The bladder is less stretchy, and there is a decreased ability to contract the urinary sphincter. If the pelvic floor muscles are weak and do not control the sphincter well, urine can leak.
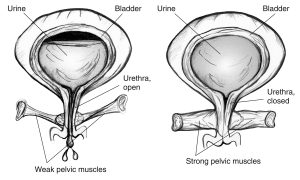 Image courtesy of National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health.
Image courtesy of National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health.
In stress incontinence, the bladder is pressed on by the abdominal muscles with coughing, sneezing, exercising, lifting, laughing etc. When the pelvic floor muscles and urinary sphincter are strong, there is an involuntary muscle contraction that prevents leaks. Stress incontinence happens when the muscles are weak or if the involuntary contraction does not happen when there’s pressure on the bladder. Studies show that women who are continent (don’t leak) have stronger pelvic floor muscles and faster contractions than women who are incontinent. Risk factors for stress incontinence include increasing age, vaginal delivery (as compared to having a C-section or no childbirth), excess body weight, prior pelvic surgery, and smoking.
Overactive bladder is the result of bladder spasms (abnormally strong bladder contractions). The spasms cause urinary urgency – feeling like you need to urinate NOW. You may also need to urinate more often. More than 8 times in 24 hours is considered too high. The spasms can also cause the urge to urinate at night also called nocturia). The spasms may or may not cause leakage. In fact, most people with overactive bladder have that sense of urgency and urinate more frequently but are not incontinent. The two biggest risk factors for overactive bladder are increasing age and excess body weight. Other things that can cause it include caffeine, alcohol, drinking a lot of fluids, some drugs, weak pelvic floor muscles, chronic constipation, and nerve damage.
Urge incontinence happens when the bladder spasms and, despite your effort to hold it in, urine leaks out. The contraction is so strong that it overrides the sphincter muscles that usually hold urine back. Many things can cause these contractions including bladder irritation and nerve damage from chronic diseases such as diabetes or Parkinson’s disease. Other risk factors for urge incontinence include older age, having had a C-section, and excess body weight.
Researchers are still studying the relationship between perimenopause and the lower urinary tract. The decrease in estrogen during perimenopause may be important because there are estrogen receptors throughout the lower urinary tract. However, after a lot of research, we know that estrogen pills can make urinary symptoms worse. In sum, there are still mysteries surrounding the way declining levels of estrogen during perimenopause affect the urinary tract. On-going research may lead to new treatments.
WHAT TO EXPECT
Women have urinary incontinence much more often men. It is more likely to emerge during pregnancy, after birth, or during perimenopause.
You may have had stress incontinence towards the end of a pregnancy, when the baby feels like it’s taking up so much room and pressing on your bladder. Those leaks when moving suddenly, coughing, sneezing, etc., typically clear up after the baby is born. Or, your pelvic floor muscles may be weaker after the birth of your child, making it more likely you will experience incontinence as you age. Your OB/GYN or midwife may have suggested that you do Kegel exercises to strengthen your pelvic floor muscles, and we recommend them, too (see below).
Aging also causes the pelvic floor muscles to weaken, just like other muscles.
Thus, both aging and perimenopause are risk factors for incontinence. More women report that urinary incontinence began after menopause than before it.
Incontinence can also be caused by other conditions, including spinal injury, stroke, diabetes, and multiple sclerosis.
Urinary incontinence and overactive bladder do not clear up on their own. In fact, they increase with age.
Treatments that are inappropriate or have not been studied for this symptom are not listed.
Please scroll beyond “References” to access more resources if you are browsing on mobile or tablet
Kegels and bladder retraining are supported by research, and are recommended. There have been studies of pilates, other abdominal exercises, and yoga as treatments for urinary incontinence, but systematic reviews found that the quality was not good enough to recommend them as treatments (Bø & Herbert, 2013, Wieland et al., 2019). Bø & Herbert (2013) also said there were no randomized control trials of Tai Chi, posture correction, breathing exercise, and general fitness training.
Alperin, M., Burnett, L., Lukacz, E., & Brubaker. 2019. The mysteries of menopause and urogynecologic health: Clinical and scientific gaps. Menopause, 26(1): 103-111. doi:10.1097/GME.0000000000001209.
Bø K, Herbert RD. There is not yet strong evidence that exercise regimens other than pelvic floor muscle training can reduce stress urinary incontinence in women: a systematic review. J Physiother. 2013 Sep;59(3):159-68. doi: 10.1016/S1836-9553(13)70180-2. PMID: 23896331.
Cody JD, Jacobs ML, Richardson K, Moehrer B, Hextall A. Oestrogen therapy for urinary incontinence in post-menopausal women. Cochrane Database Syst Rev. 2012 Oct 17;10(10):CD001405. doi: 10.1002/14651858.CD001405.pub3. PMID: 23076892; PMCID: PMC7086391.
Dumoulin C, Cacciari LP, Hay Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews 2018, Issue 10. Art.No.: CD005654. DOI: 10.1002/14651858.CD005654.pub4.
Fu, Y., Nelson, EA, & McGowan, L. 2019. Multifaceted self-management interventions for older women with urinary incontinence: A systematic review and narrative synthesis. BMJ Open 2019;9:e028626. doi:10.1136/bmjopen-2018-028626
Keating KN, Perfetto EM, Subedi P. Economic burden of uncomplicated urinary tract infections: direct, indirect and intangible costs. Expert Rev Pharmacoecon Outcomes Res 2005;5:457–466. [PubMed: 19807263]
Kinchen KS, Lee J, Fireman B, Hunkeler E, Nehemiah JL, Curtice TG. The prevalence, burden, and treatment of urinary incontinence among women in a managed care plan. J Womens Health (Larchmt). 2007;16:415-22. [PMID: 17439386]
Losada, (2016). Expert Panel Recommendations on Lower Urinary Tract Health of Women Across Their Life Span: Report from the Society for Women’s Health Research. Journal of Women’s Health. Volume 25, Number 11. DOI: 10.1089/jwh.2016.5895.
Qassem et al. Nonsurgical Management of Urinary Incontinence in Women: A Clinical Practice Guideline From the American College of Physicians. 2014. Annals of Internal Medicine 161 (6): 429-440. https://doi.org/10.7326/M13-2410
Rahn DD, Carberry C, Sanses TV, Mamik MM, Ward RM, Meriwether KV, Olivera CK, Abed H, Balk EM, Murphy M; Society of Gynecologic Surgeons Systematic Review Group. Vaginal estrogen for genitourinary syndrome of menopause: a systematic review. Obstet Gynecol. 2014 Dec;124(6):1147-1156. doi: 10.1097/AOG.0000000000000526. PMID: 25415166; PMCID: PMC4855283.
Stewart, F., Berghmans, B., Bø, K., Glazener, C. Electrical stimulation with non-implanted devices for stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2017. DOI: https://doi.org/10.1002/14651858.CD012390.PUB2
Vissers, D., Neels, H., Vermandel, A., De Wachter, S., Tjalma, W.A.A., Wyndaele, J.‐J. and Taeymans, J. (2014), Weight loss and urinary incontinence. Obes Rev, 15: 610-617. https://doi.org/10.1111/obr.12170
Wieland LS, Shrestha N, Lassi ZS, Panda S, Chiaramonte D, Skoetz N. Yoga for treating urinary incontinence in women. Cochrane Database Syst Rev. 2019 Feb 28;2(2):CD012668. doi: 10.1002/14651858.CD012668.pub2. PMID: 30816997; PMCID: PMC6394377.
Authors: Dr. Leslie Snyder & Dr. Katherine Newton. Last reviewed: April, 2021.